RESET THE BODY'S IMMUNE SETPOINT

Many diseases, one common cause: chronic inflammation
There is established evidence that chronic inflammation plays a role in causing and advancing many autoimmune diseases including rheumatoid arthritis (RA), inflammatory bowel disease (IBD), psoriasis, and multiple sclerosis.1,2,3 The immune system plays a critical role in fighting infection and maintaining a balanced state in inflammatory pathways. Recent discoveries have indicated vagus-nerve mediated pathways play a significant role in maintaining this balance,2,3,4 and their dysfunction may be contributing to uncontrolled inflammation.5,6
Significant advances in immunology, neuroscience, and engineering have converged to create a groundbreaking new treatment approach: Neuroimmune Modulation.
The Evolution of Neuroimmune Modulation
Dr. Kevin Tracey publishes first ever use of TNF antibodies to reduce systemic inflammation in baboon model of acute septic shock.
Dr. Feldmann and Dr. Maini publish the use of TNFi antibodies for treatment of RA.
Infliximab is first biologic approved for Crohn’s Disease and RA.
Dr. Tracey hypothesizes that vagus nerve stimulation can reduce systemic inflammation.1
SetPoint Medical founded
Dr. Charlie Serhan discovers classes of immunoresolving lipidomics linked to vagus nerve.
First Proof of Concept study to evaluate neuroimmune modulation in RA disease activity with implantable device.5
Researchers from Academic Medical Center in Amsterdam publish that autonomic dysfunction precedes development of clinical RA.
Pilot study demonstrates feasibility of SetPoint System in RA patients.6
Large, randomized controlled pivotal trial, RESET-RA study proves safety and effectiveness of SetPoint System for treatment of biologic-experienced RA.
SetPoint System is FDA-approved for adults with moderately to severely active RA and inadequate response or intolerance to one of more biologics or JAK inhibitors.
The neuroimmune connection
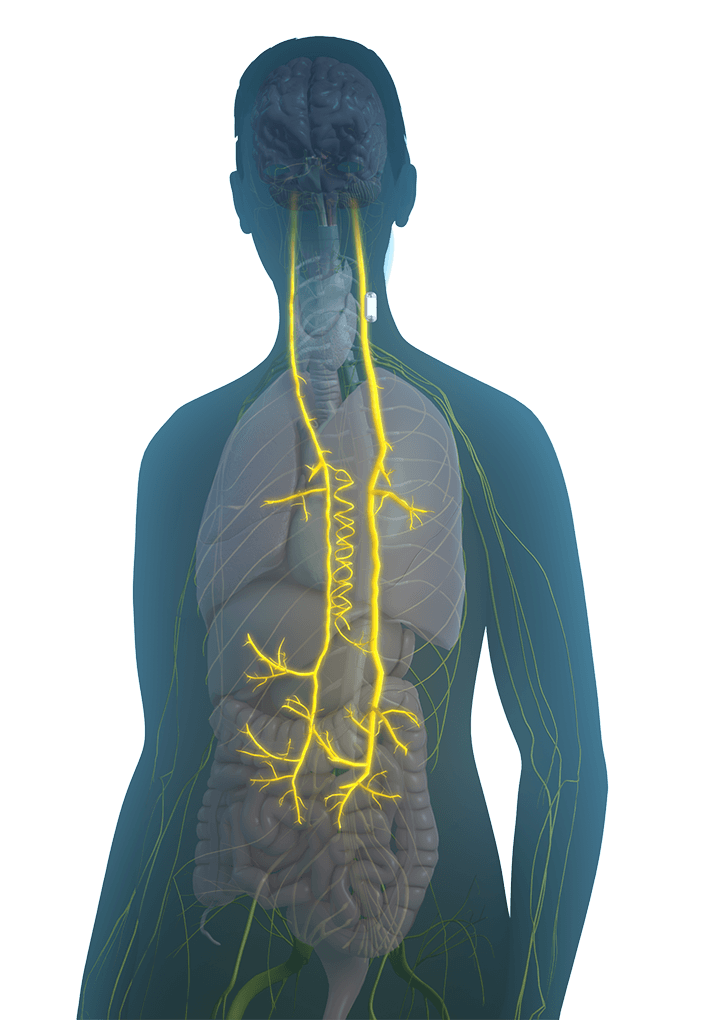
The vagus nerve is the longest cranial nerve in the body and innervates many organs. It is composed of thousands of sensory and motor neurons. The sensory neurons detect and respond to inflammatory mediators by sending signals to the brainstem, where a signal reflexively originates.1,2,3 The central nervous system governs homeostatic control of both immune responses and bone turnover through these innate neuroimmune7,8,10 and osteo-targeted reflexes.4
How the science works
How does neuroimmune modulation manage inflammation?
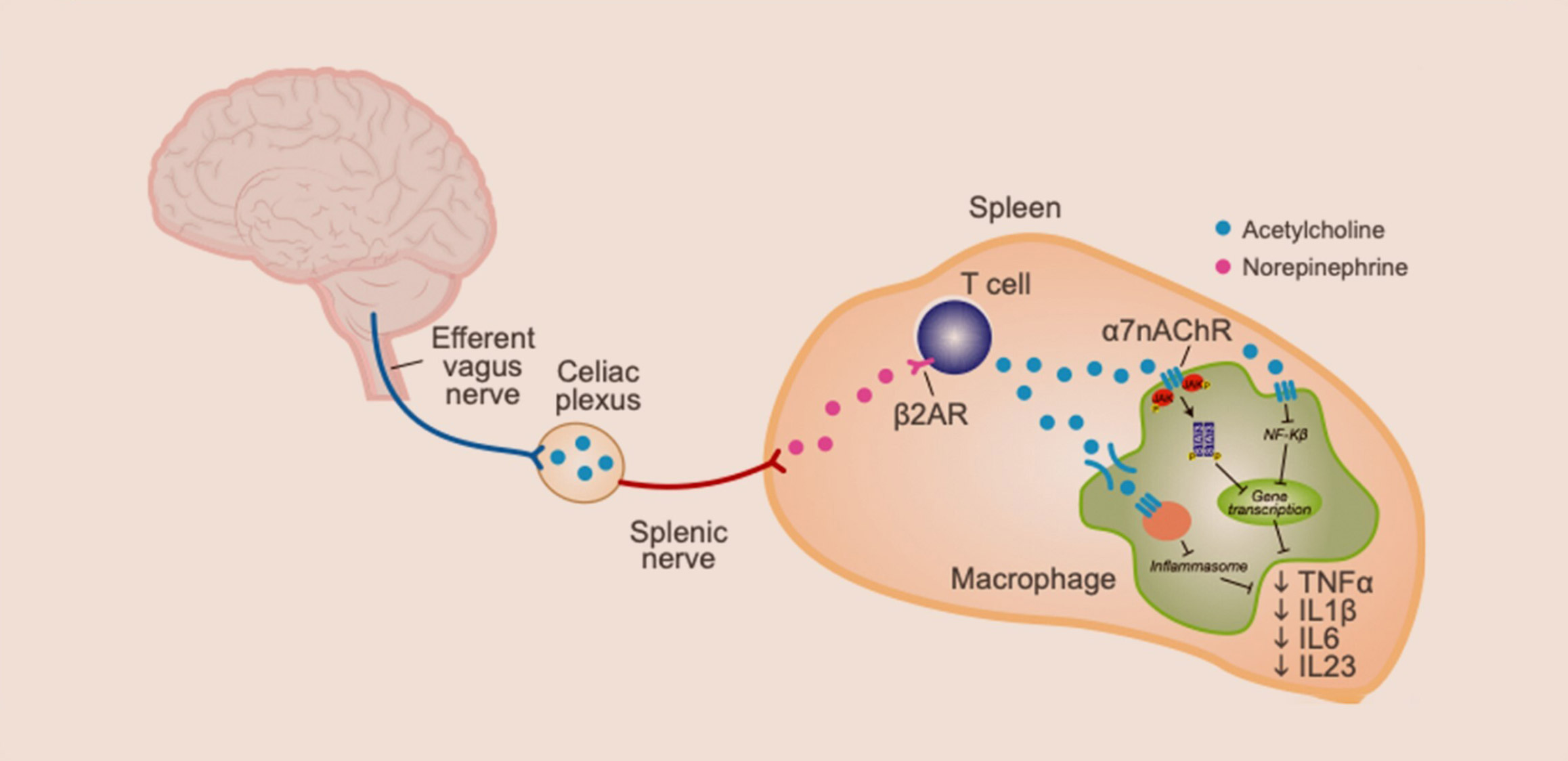
Electrically stimulating the vagus nerve with precise parameters activates specific motor pathways within the vagus nerve that transmit a signal to the splenic nerve causing the release of norepinephrine in the spleen. Specialized CD4+ T lymphocytes (T-cells) in the spleen, expressing adrenaline receptors, take up the norepinephrine and release acetylcholine, which in turn binds to the α7 nicotinic receptors on immune cells. 2,3,4 Subsequent modulation of intracellular processes acting through NFkB, JAK/STAT, and the inflammasome leads to reduced production of an array of proinflammatory cytokines like TNF, IL-6, IL-1β. 4,5,6 This broad-spectrum immunomodulation retains cytokine network bioavailability, thereby allowing reduction of inflammation while maintaining competent immunosurveillance against foreign pathogens and precancerous cells.3,4,12
How does neuroimmune modulation protect joints?
Further, electrical stimulation of the vagus nerve induces release of specialized pro-resolving mediators and neurotransmitters that signal through specific receptors including the ChemR23 receptors, acetylcholine receptors and adrenergic receptors on osteoblasts, osteoclasts, and osteocytes resulting in reduction of osteoclastogenesis and osteoclastic activity.7,8,10 This mechanism is thought to provide a protective effect on bone mediated by the canonical RANKL/osteoprotegerin pathway as well as direct effects on osteoblasts and osteoclasts. 7,11
SetPoint Medical’s breakthrough
With these discoveries, SetPoint Medical’s researchers set out to characterize these anti-inflammatory and immune-restorative pathways, and harness it for therapeutic use. Over the past 20 years, we identified the specific fibers in the vagus nerve and defined the precise stimulation parameters to activate these reflexes.
Biomarker analysis indicated that the anti-inflammatory response through a single one-minute stimulation lasted more than 24 hours.1,2 More importantly, this approach suppressed inflammatory cytokines by 30-70%5,6 without eliminating their bioavailability, thereby reducing inflammation with the potential to be less immunosuppressive.3,12
The SetPoint System is specifically designed to activate the body’s immunomodulatory pathways with targeted electrical stimulation to regulate inflammation and restore immunologic balance in people living with RA.
Advancing the possibilities
SetPoint Medical has studied its neuroimmune modulation therapy for treatment of various inflammation-mediated immune diseases, including rheumatoid arthritis and inflammatory bowel disease, specifically Crohn’s disease.
While the SetPoint System is currently only indicated for treatment of biologic-experienced RA, we continue our evidence-based advancement of this therapeutic approach for other chronic autoimmune diseases, including relapsing remitting multiple sclerosis (RRMS).
Latest publications
Ready to get activated?
2. van Maanen MA, et al. The cholinergic anti-inflammatory pathway: towards innovative treatment of rheumatoid arthritis. Nat Rev Rheumatol. 2009;5(4):229-232.
3. Kelly MJ, et al. Manipulation of the inflammatory reflex as a therapeutic strategy. Cell Rep Med. 2022;3(7):100696.
4. Chavan SS, et al. Mechanisms and Therapeutic Relevance of Neuro-immune Communication. Immunity. 2017;46(6):927-942
5. Koopman FA, et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc Natl Acad Sci U S A. 2016;113(29):8284-8289.
6. Genovese MC, et al. Safety and efficacy of neurostimulation with a miniaturised vagus nerve stimulation device in patients with multidrug-refractory rheumatoid arthritis: a two-stage multicentre, randomised pilot study. Lancet Rheumatol. 2020;2(9):e527-e53
7. van Maanen MA, et al. The alpha7 nicotinic acetylcholine receptor on fibroblast-like synoviocytes and in synovial tissue from rheumatoid arthritis patients: a possible role for a key neurotransmitter in synovial inflammation. Arthritis Rheum. 2009;60(5):1272-1281.
8. Elefteriou F. Impact of the Autonomic Nervous System on the Skeleton. Physiol Rev. 2018;98(3):1083-1112.
9. Serhan CN, et al. Novel mediators and mechanisms in the resolution of infectious inflammation: evidence for vagus regulation. J Intern Med. 2019;286(3):240-258.
10. Bajayo A, et al. Skeletal parasympathetic innervation communicates central IL-1 signals regulating bone mass accrual. Proc Natl Acad Sci U S A. 2012;109(38):15455-15460.
11. Ali M, et al. Application of specialized pro-resolving mediators in periodontitis and peri-implantitis: a review. Eur J Oral Sci. 2021;129(1):e12759.
12. Levine YA, et al. Harnessing the Inflammatory Reflex for the Treatment of Inflammation-Mediated Diseases. Cold Spring Harb Perspect Med. 2020;10(1):a034330.


